How Fluidity Rx Helps With Pelvic Pain
Explore Fluidity Rx- Fluidity Rx helps with proportional strength by training the pelvic floor muscles (PFMs) for coordination and relaxation, and by balancing the pelvic girdle (spine, pelvis, and hips) for both flexibility and strength.
- Fluidity Rx develops pelvic floor muscles (PFMs), inner core, and abdominal wall strength and endurance which are key to maintaining functional pain-free movement. Fluidity Rx promotes effective blood flow and venous return in the abdomen and pelvis.
Pelvic Pain Dysfunctions Supported By Fluidity Rx
Pelvic pain, pelvic floor dysfunction PFD is typically a problem of overactive pelvic floor muscles (PFMs) — the pelvic floor muscles (PFMs) may respond to painful conditions by increasing activity and tension.
- Pelvic floor myofascial pain — increased pelvic floor muscle tension
- Sacroiliac joint dysfunction (pelvic girdle joint pain)
- Levator Ani Syndrome
- Pubic Symphysis Dysfunction (PSD)
- Vaginismus (spasm of the superficial PFM)
- Coccydynia (tailbone pain)
- Anismus (spasm of the anal sphincter)
- Polycystic Ovary Syndrome (PCOS)
- Recurrent urinary tract infections (UTIs)
- Proctalgia Fugax (random rectal pain)
- Dysmenorrhea (painful periods)
- Pudendal Neuralgia (nerve pain of the main nerve to the PFM and vagina)
- Endometriosis pain
- Vestibulodynia / Vulvodynia (severe hypersensitivity of the tissues of the vaginal opening)
- Dyspareunia (painful intercourse)
- Dysorgasmia (painful orgasm)
- Pelvic venous disease
- Prostatitis (non-bacterial Type IV)
- Endometriosis pain
- Interstitial cystitis / Bladder Pain Syndrome
- Chronic Pelvic Pain Syndrome (CPPS)
- Perineal Injury and Discomfort
How Misaligned Pelvic Tilts Lead to Pelvic Pain
A misaligned pelvis disrupts the structural harmony of the pelvic basin, placing uneven stress on joints, muscles, and fascia. This imbalance can compress nerves, strain the sacroiliac joints, and create asymmetrical tension across the pelvic floor, leading to chronic pain, instability, and difficulty with movement.
1
2
3
4
A Neutral Pelvis is Essential to Resolve Pelvic Pain
A neutral pelvis restores structural harmony across the spine, hips, and pelvic floor, allowing muscles and fascia to engage symmetrically without compensatory tension. This alignment reduces joint compression, improves circulation, and supports reflexive core activation—key factors in resolving chronic pelvic pain. By optimizing load transfer and nerve signaling, a neutral pelvis creates the conditions for healing rather than perpetuating dysfunction.
Your Core The Inner Unit
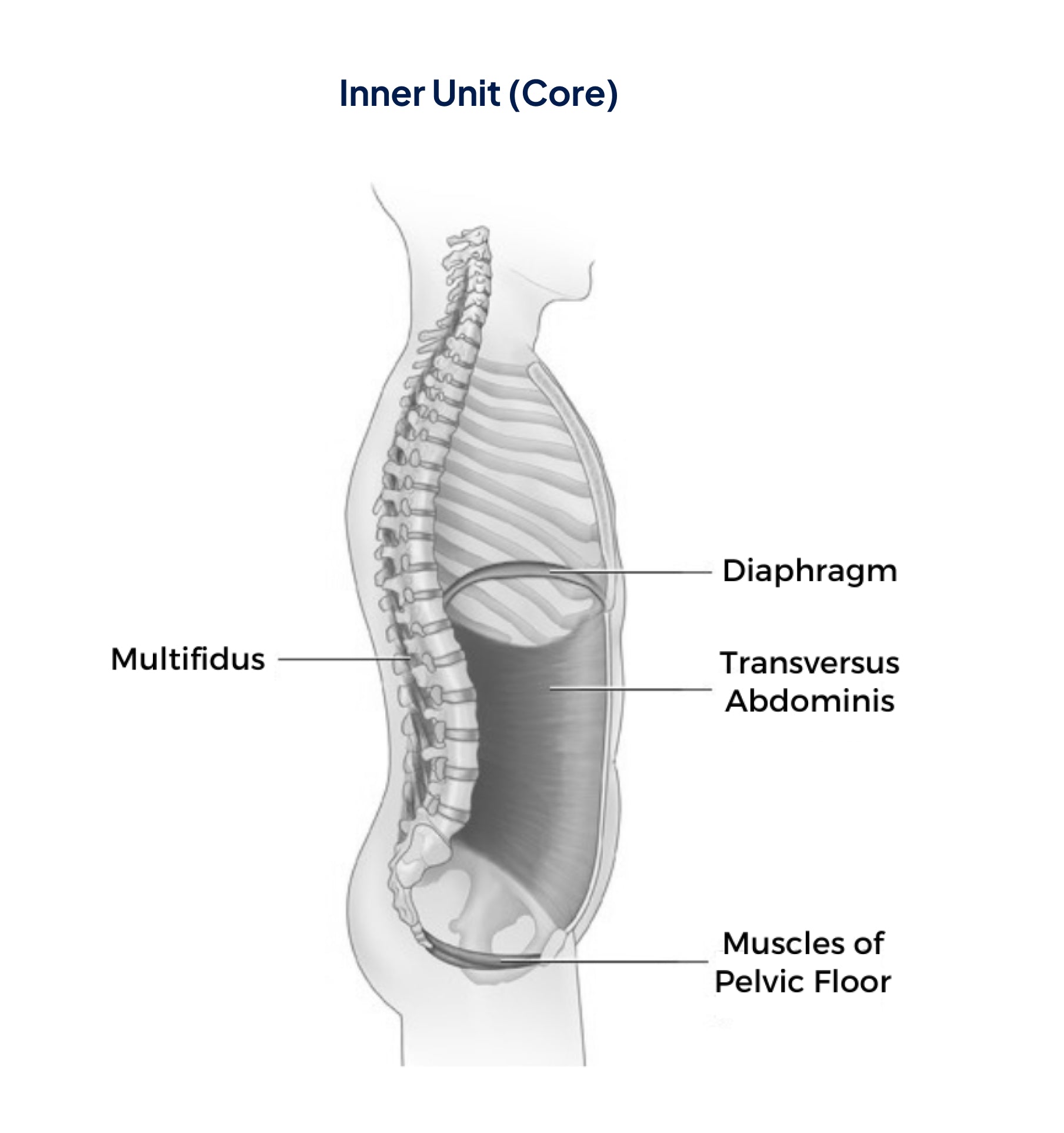
The Inner Unit automatically activates to:
- Control intra-abdominal pressure (the pressure in the abdomen between the lungs and the pelvic floor)
- Stabilize the spine and pelvis before you move your arms and/or legs during movement
When intra-abdominal pressure (IAP) is functioning optimally, It
- Helps Stabilizes the Spine and Core
- Coordinates Breathing and Movement
- Enhances Strength and Ensures Coordinated Force Distribution from the Torso to the Limbs.
- Supports Pelvic Floor and Organ Function.
- Promotes Postural Alignment

“Fluidity Rx provides the optimal method for not only pelvic floor muscle training but also to incorporate the pelvic floor muscles functionally into optimal movement patterns. Fluidity Rx training maximizes a person’s ability to modulate intra-abdominal pressure by the precise training of co-contraction of the pelvic floor with the abdominal, spine, and diaphragm muscles for inner core muscle strength.”
Dr. Cindy Neville
PT, DPT, WCS
Women with Stress Urinary Incontinence are 17 times more likely to heal if they strengthen their pelvic-floor muscles [1]
Women with Stress Urinary Incontinence are 17 times more likely to heal if they strengthen their pelvic-floor muscles [1]
















