How Fluidity Rx Helps With Pelvic Organ Prolapse (POP)
- Fluidity Rx helps with Pelvic Organ Prolapse (POP) by training the pelvic floor muscles for power, endurance, and coordination so that they support the pelvic organs, especially during activities which increase intra-abdominal pressure and can cause strain.
- Fluidity Rx trains the Pelvic Floor Muscles to respond to and control this pressure to minimise and prevent excessive strain on organs and the connective tissue support system.

For Women
- Pelvic organ prolapse occurs in women when the internal connective tissue architecture between the organs of the bladder and/or urethra and vagina, rectum and vagina, small intestine and vagina, or uterus and vagina loses its ability to hold the organs in their typical position in the pelvis. The organs herniate or “bulge” from their normal position through the weakened connective tissue and into the vagina.
- POP is often an under-active Pelvic Floor Dysfunction (PFD), but also can be an overactive PFD or incoordination PFD.
Most Common Types
Rectocele
- Rectum bulges into the posterior vaginal wall through the rectovaginal septum.
Cystocele
- Bladder bulges into the anterior vaginal wall due to weakened fascia (most common).
Enterocele
- Small intestine herniates into the vaginal canal, typically post-hysterectomy.
Urethrocele
- Urethra descends into the vaginal canal, often co-occurs with cystocele.
Vaginal Vault Prolapse
- Top of the vaginal canal descends, especially after hysterectomy.
Cystourethrocele
- Combined descent of bladder and urethra into the vagina.
Uterine Prolapse
- Uterus descends into or outside the vaginal canal, often due to ligament laxity.
Examples of Pelvic Organ Prolapses
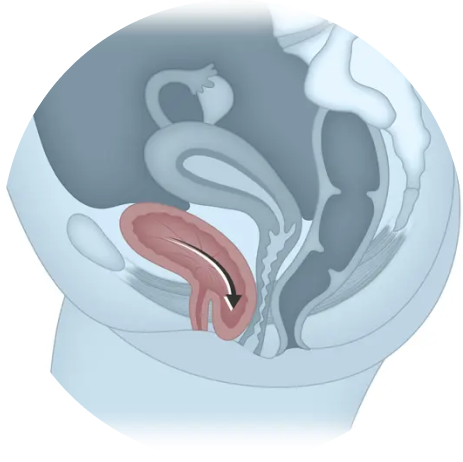
Cystocele (Bladder Prolapse)

Rectocele(Rectum Prolapse)
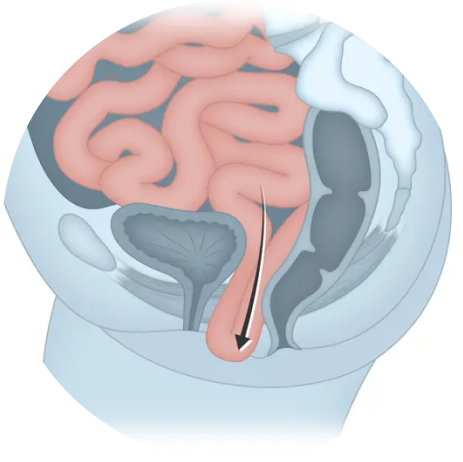
Enterocele (Small Intestine Prolapse)
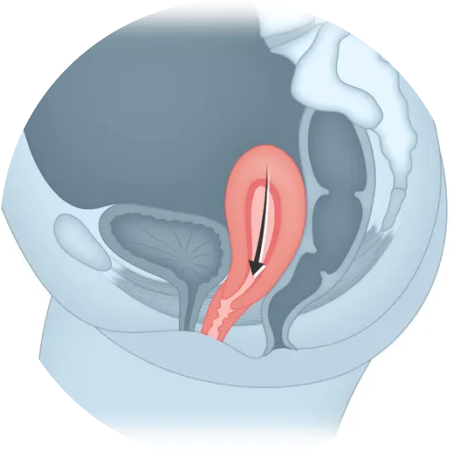
Uterine or Vaginal Apex Prolapse
© IHH Healthcare Singapore
For Men
- Pelvic organ prolapse in men occurs when the internal connective tissue architecture that supports the bladder, urethra, rectum, and small intestine loses its ability to maintain these organs in their typical anatomical positions within the pelvis. This weakening may involve the levator ani muscles, endopelvic fascia, and perineal body, which together form the structural support system beneath and around the pelvic organs.
- When this support system deteriorates—due to aging, chronic straining, neurological injury, or surgical disruption—the affected organs may herniate or “bulge” through the compromised connective tissue and into adjacent compartments. In severe cases, the rectum may protrude externally through the anus (rectal prolapse), or the bladder and urethra may descend toward the perineum, contributing to urinary dysfunction.
Most Common Types
of Prolapse in Men
Bladder Descent
- Bladder drops toward the perineum, often post-prostatectomy. May cause urinary retention, leakage, or frequency.[2]
Rectal Prolapse
- Full-thickness descent of the rectal wall through the anal canal. Most common in men, especially with chronic straining or neurological conditions.
Enterocele
- Herniation of the small intestine into the rectal or perineal space. Rare in men, but possible after pelvic surgery or with severe connective tissue failure.[1]
Perineal Descent
- Sagging of the perineum (between scrotum and anus) due to weakened pelvic floor support. Often linked to aging, constipation, or pelvic floor dysfunction.[1]
Urethral Prolapse
- Protrusion of the urethral lining through the external meatus. Extremely rare in men, typically congenital or trauma-related.[1]
How Misaligned Pelvic Tilts Empower Pelvic Organ Prolapses (POP)
Pelvic misalignment alters the structural support system of the pelvic floor, placing uneven strain on muscles, ligaments, and fascia that hold pelvic organs in place. This imbalance weakens the hammock-like support beneath the bladder, uterus, and rectum, allowing them to descend or bulge into the vaginal canal in women. In men, pelvic misalignment can contribute to prolapse of the bladder, rectum, or even the prostate by weakening the connective tissue and muscular support structures that stabilize these organs.
1
2
3
4
A neutral pelvic is an ideal predisposition to prevent and mitigate Pelvic Organ Prolapses (POP)
A neutral pelvis helps prevent and mitigate pelvic organ prolapse in all genders by restoring optimal alignment and muscular balance across the pelvic floor. This positioning allows the muscles, ligaments, and fascia to support the bladder, rectum, and reproductive organs without excessive strain or downward pressure. By improving load transfer, nerve signaling, and intra-abdominal pressure regulation, a neutral pelvis reduces the risk of organ descent and promotes tissue resilience—supporting healing and preventing further prolapse.
Your Core The Inner Unit
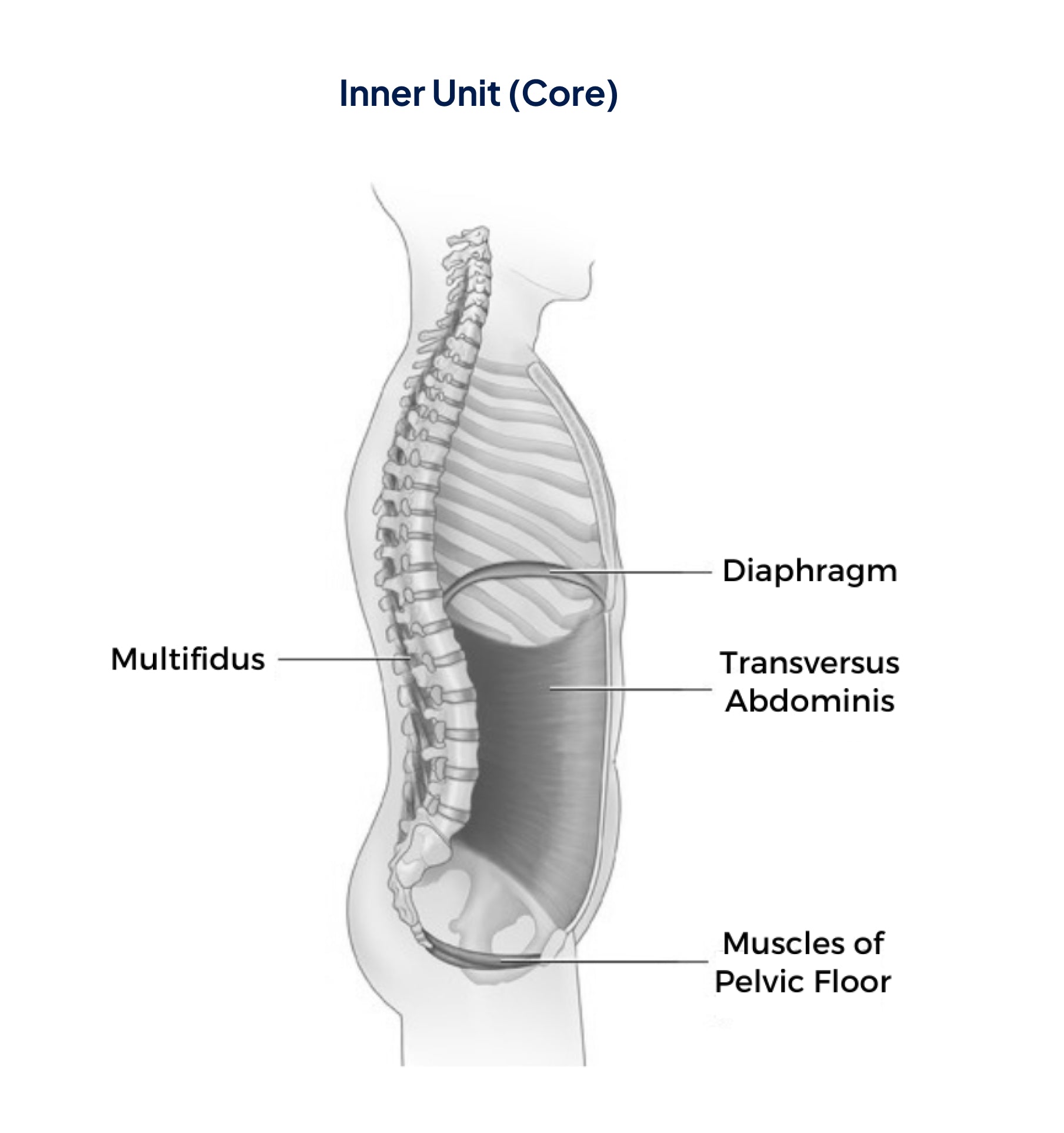
The Inner Unit automatically activates to:
- Control intra-abdominal pressure (the pressure in the abdomen between the lungs and the pelvic floor)
- Stabilize the spine and pelvis before you move your arms and/or legs during movement
When intra-abdominal pressure (IAP) is functioning optimally, It
- Helps Stabilizes the Spine and Core
- Coordinates Breathing and Movement
- Enhances Strength and Ensures Coordinated Force Distribution from the Torso to the Limbs.
- Supports Pelvic Floor and Organ Function.
- Promotes Postural Alignment

“Fluidity Rx provides the optimal method for not only pelvic floor muscle training but also to incorporate the pelvic floor muscles functionally into optimal movement patterns. Fluidity Rx training maximizes a person’s ability to modulate intra-abdominal pressure by the precise training of co-contraction of the pelvic floor with the abdominal, spine, and diaphragm muscles for inner core muscle strength.”
Dr. Cindy Neville
PT, DPT, WCS
Women with Stress Urinary Incontinence are 17 times more likely to heal if they strengthen their pelvic-floor muscles [1]
Women with Stress Urinary Incontinence are 17 times more likely to heal if they strengthen their pelvic-floor muscles [1]
















